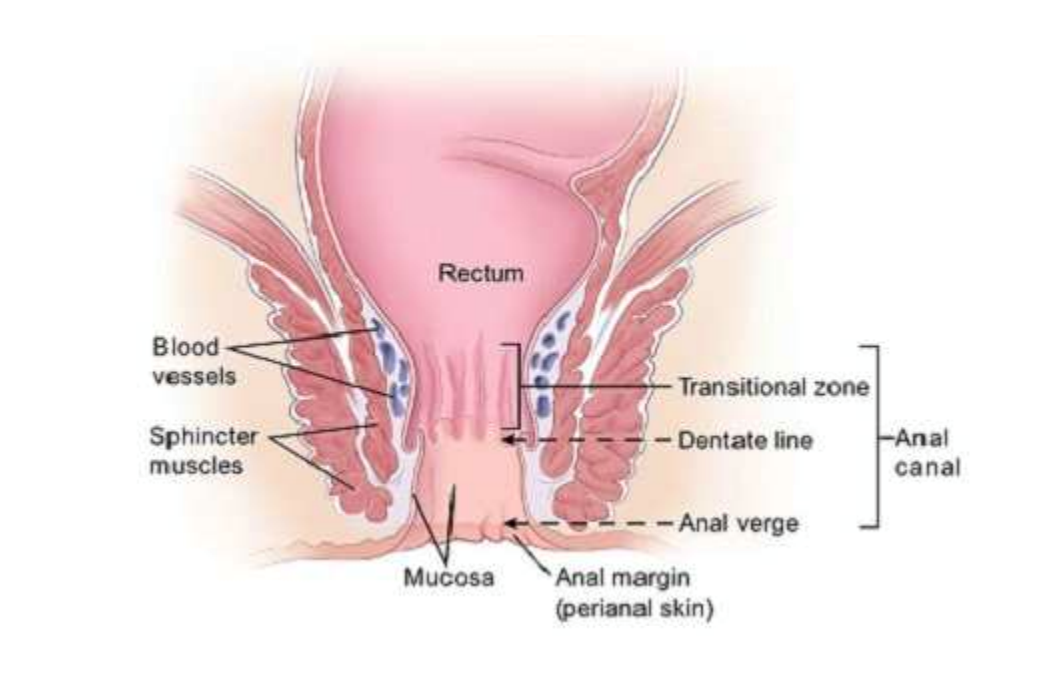
Anal cancer is defined as a cancer arising either from the squamous or glandular epithelium of the anus. The vast majority are SCCs (36), with the remainder coded as adenocarcinomas, neuroendocrine neoplasm, malignant melanoma, mesenchymal tumours and lymphoma (36-39). Anal cancers are distinguished anatomically as being of the anal canal (arising from the canal which extends between the rectum to perianal skin) or perianal (arising from the skin within 5 cm diameter from the anal verge) (Figure 3).
Figure 3. Anatomy of the anal canal (40)
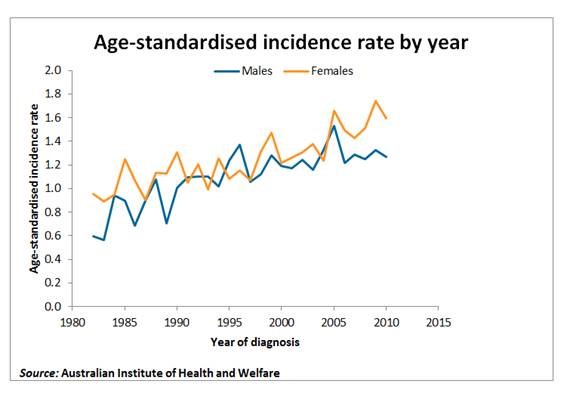
Anal cancer is relatively rare in the general population with incidence rates between 1 to 2 per 100,000 person-years, though rates are rising over time (Figure 4) (36, 38, 41-43). However, for men who have sex with men (MSM) who have HIV infection, a recent meta-analysis estimated a pooled incidence rate of 77.8 per 100,000 person-years (44). This is comparable with other common cancers in the general Australian population (45).
Figure 4. Australian age-standardized incidence rate of anal cancer by gender (43)
Squamous cell carcinoma is the commonest (85%) form of anal cancer and is primarily caused by HPV infection (46-49). Additional risk factors are receptive anal intercourse (before the age of 30) (49-51), higher lifetime number of sexual partners (50, 51), current cigarette smoking (48, 52, 53), genital warts (50, 53), and immunosuppression (HIV, post-organ transplantation) (49, 54-56). Anal fistulae and epithelial trauma may also be associated, possibly because they increase access of HPV to the basement membrane (57-59).
An increased incidence of anal cancer in the last 30 years has been attributed to changes in sexual behavioural patterns (60, 61), including increased anal sex (61, 62) and increased partner numbers for both MSM and women, as well as the increased number of people with HIV infection (63). A recent cancer registry study in the United Kingdom has shown a 126% increase of anal carcinoma incidence in women comparing the time periods 2006-2010 to 1990-1994; whereas in men the increase was only 69% with the male to female ratio being 10:18 (64).
Screening
There are no consistent guidelines on how to screen for anal cancer or pre-cancerous lesions. If available, anal cytology with or without high resolution anoscopy has been recommended to detect anal cancer precursor lesions (analogous to cervical cancer) (65). There is ongoing research (including a large randomized controlled trial in the United States) to determine the effectiveness of this screening modality.
As evidence gathers for screening using anal cytology, those people at highest risk of anal cancer are recommended to have an annual digital anorectal examination (DARE) (66-68). Early anal cancer detection is associated with better morbidity and mortality outcomes (41, 69, 70). Resources for performing DARE are available on the following websites: www.anal.org.au/clinician and https://youtu.be/KDUcJHdz-Sk.
Clinical presentation
Anal cancer may present as rectal bleeding, anal or perineal pain, a painful/hard/friable mass, pruritus ani, faecal incontinence, anal fistula, anal discharge and ulceration (71-75). Up to 80% of anal cancers may be symptomatic at the time of diagnosis (76). However, symptoms may be present at a mean time of 22 weeks before diagnosis is made (72). In a large UK cohort of 8,640 people with HIV infection (40,126 patient years of follow up), a significant majority of anal cancer cases were diagnosed late; 38% had cancers larger than 5 cm, 31% had nodal disease and 6% had distal metastases (77). In evaluating 585 anal cancer patients in the UK, only 13% of anal canal tumours and 10% of anal margin tumours were smaller than 2 cm (78). A series of 128 cases of anal cancers in Victoria reported that 52% of anal cancers were externally visible at diagnosis with a mean tumor size of 3.6 cm (72).
Diagnosis
A biopsy of any suspicious lesions should be conducted to confirm the diagnosis together with staging investigations such as CT, MRI or PET scan. For more details, see (79).
Management
Cancers of the perianal skin and those of the anal canal have different outcomes (80). Early stage perianal lesions can usually be treated by surgical excision whereas the anal canal lesions require chemoradiotherapy (79, 80). The prognosis depends on the site, size of the lesion (<2cm, 2-5cm, >5cm) and whether there is nodal involvement or metastases. The 5-year survival for anal cancer is approximately 70% (81), with a better prognosis for early disease (i.e. 70-92% 5-year survival rate for Stage I disease) (82). It is not yet known if detection at the microinvasive stage is associated with a better long-term prognosis. In people with HIV infection, anal cancer prognosis and treatment toxicities are similar to those of the general population(83).

