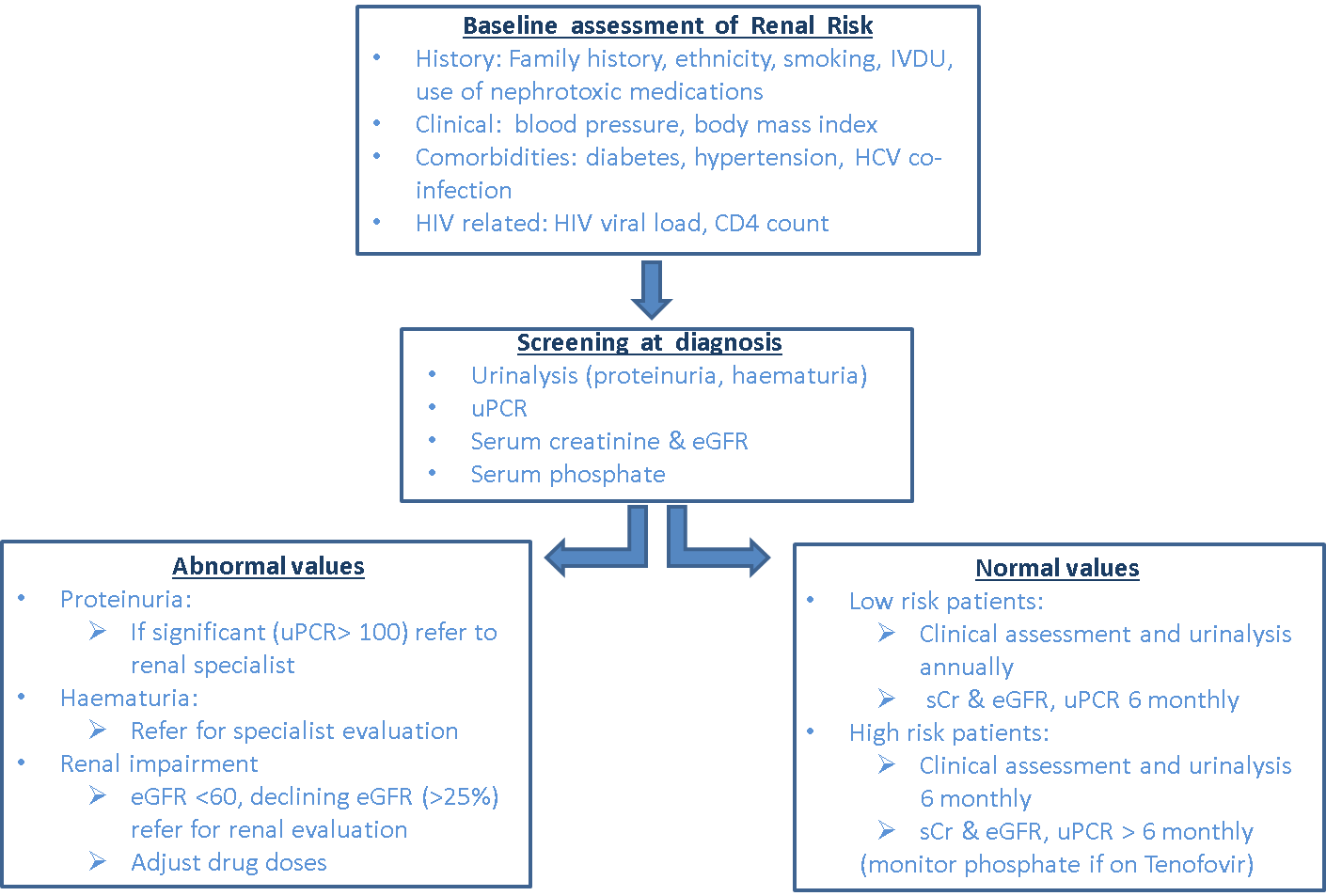
Clinically, CKD is often asymptomatic and is often detected on routine screening22. Patients who are at risk for renal disease should be routinely screened for the presence of CKD23. In addition to a full clinical assessment for risk factors for renal disease and measurement of blood pressure, at risk patients should have a urine test for albuminuria and a blood test for creatinine to estimate their renal function24.
The measurement of renal function, or the GFR, is complex and the most commonly used methods are imperfect25. The estimated GFR (eGFR) is the most widely used clinical measure of renal function. This value is derived from the level of serum creatinine, a breakdown product of muscle metabolism. The serum creatinine level is not an ideal measure of GFR, as creatinine is both filtered by the glomerulus and actively excreted by proximal renal tubular cells26. Therefore, medications interfering with the excretion of creatinine may alter the serum creatinine level, without an actual change in GFR. This has implications for some antiretroviral drugs, which can interfere with the tubular transport of creatinine. As well, the serum creatinine level is determined by muscle mass and so varies by sex, race, age and body mass index. The serum creatinine level must be interpreted mindful of these individual patient factors27,28.
Urinalysis, or the urine dipstick, is used to detect proteinuria, as well as to provide information regarding other markers of renal pathology, such as haematuria and glycosuria. The urine dipstick predominantly detects albuminuria, a hallmark of glomerular disease, and may not detect other urinary proteins. This characteristic is important, as other proteins may predominate in certain clinical situations, such as tubular proteinuria, which may be seen with the use of tenofovir disoproxil fumurate (TDF)29. Therefore, a urinary protein:creatinine ratio (uPCR) is preferable in patients with HIV infection, particularly those patients receiving TDF. As well, patients receiving TDF may have abnormalities of their serum phosphate level; a low serum phosphate level may be seen with proximal tubular dysfunction30.
Screening for renal disease
International guidelines recommend that HIV-infected patients should be screened regularly for CKD to allow for its early detection and prompt management21,29. Because of the high risk of CKD in this patient group, it is recommended that these patients have their GFR estimated at least every 6 months and should have either a urinalysis or a quantitative assessment of their urinary protein excretion at least annually. Patients whose eGFR has declined by 25% or more, or to a level below 60mL/min/1.73m2, or who have protein excretion of over 300mg/day, should be referred for evaluation by a Nephrologist29. Patients who are found to have haematuria with any level of proteinuria or GFR should also be referred for assessment.
In patients receiving TDF, it is recommended that the serum phosphate level be monitored and that more frequent screening for CKD is undertaken30. An Australian consensus statement regarding the monitoring of patients receiving TDF suggested that patients be tested at baseline for serum creatinine, eGFR, serum phosphate level, urinalysis and assessment of the uPCR. Repeat screening was suggested at 3-monthly intervals for the first year of therapy and then at least annually in all patients; more frequently if any abnormalities are detected30.
Adherence to accepted guidelines for screening for CKD in HIV-infected patients is variable16. A suggested approach to screening for renal disease in patients with HIV is shown in Figure 1.
Figure 1. Screening for renal risk in patients with HIV infection (adapted from Holt et al30., Lucas et al21. and European AIDS Clinical Society [EACS] guidelines29).