HLA-B27 associated disease
HIV positive individuals can get severe anterior uveitis as part of a systemic HLA-B27 related illness or as isolated HLA-B27 related ocular disease. HLA-B27 related anterior uveitis can occur as part of a HLA-B27 related reactive disease triggered by gram negative bacterial gut infection or chlamydial genito-urinary infection.
Keratouveitis
Varicella Zoster Virus keratouveitis
Varicella Zoster Virus (VZV) keratouveitis is common in HIV-infected patients, with or without the typical dermatomal rash of Herpes Zoster Ophthalmicus (HZO). VZV is a dsDNA virus of the herpes group. Primary infection of VZV results in chickenpox (varicella). Reactivation of virus dormant in the sensory ganglion results in shingles (herpes zoster) of the innervated dermatome. Involvement of the ophthalmic branch of the trigeminal nerve (Cranial nerve Va) occurs in 25% of shingles cases and results in HZO (Figure 1). VZV infection may be more severe in the immunosuppressed {ref} Singalavanija T, Ausayakhun S, Tangmonkongvoragul C. Anterior segment and external ocular disorders associated with HIV infections in the era of HAART in Chiang Mai University Hospital, a prospective descriptive cross sectional study. PLoS One. 2018;13(2){/ref}
Figure 1. Right nasociliary nerve involvement in Herpes Zoster Ophthalmicus.

Source: Uveitis Department, Sydney Eye Hospital, with permission.
Clinical features of HZO include a viral prodrome, preherpetic neuralgia (mild intermittent tingling to severe constant electric pain), rash (papules, vesicles, pustules, scabs) predominantly within the one dermatome (Cranial nerve Va); Hutchinson’s sign (cutaneous involvement of the tip of the nose, indicating nasociliary nerve involvement and increased likelihood of ocular involvement); it may be disseminated (involving multiple dermatomes) in immunocompromised patients {ref} Bowling B. Kanski's Clinical Ophthalmology, 8th Edition - A Systematic Approach. England: Saunders Ltd; 2015. 928 p {/ref}
Once the cornea becomes involved there can be epithelial involvement, stromal nummular keratitis with anterior stromal granular deposits, necrotizing keratitis with stromal infiltrates, thinning, and even perforation. Disciform endotheliitis, Descemet’s folds, anterior uveitis and Keratic Precipitates (KPs - an inflammatory cellular deposit seen on the corneal endothelium) can also occur (Figure 2). Neurotrophic changes can occur with corneal nerve damage causing persistent epithelial defects, thinning, and even perforation. Mucus plaques with linear grey elevations, loosely adherent to underlying diseased epithelium/ stroma can occur later on and be chronic. Laboratory investigations include obtaining a sample of vesicle fluid in viral transport media for VZV nucleic acid testing by PCR. Initial systemic treatment includes antivirals, which should be commenced as soon as the rash appears (Table 3).
Table 3. Directed treatment for anterior segment opportunistic infections
|
Condition |
Treatment |
Duration |
|
VZV keratouveitis |
Valaciclovir 1g orally q8h OR Famciclovir 500mg orally q8h OR Aciclovir 800mg orally 5 times daily OR Aciclovir 10mg/kg/day intravenously |
7 to 14 days |
|
HSV keratouveitis |
Valaciclovir 1g orally q12h OR Famciclovir 500mg orally q12h OR Aciclovir 800mg orally 3 times daily OR Aciclovir 10mg/kg/day intravenously |
7 to 10 days |
Post-herpetic neuralgia may cause depression (sometimes resulting in suicide). Treatments include amitriptyline and gabapentin. Viral reactivation, replication, and retrograde migration to the cornea results in recurrent keratitis, which may be epithelial, stromal, endothelial (discoid), or neurotrophic. Potential intraocular involvement includes anterior uveitis and retinitis. Additionally, the resultant neurotrophic cornea is vulnerable to bacterial and fungal keratitis. Depending on which layer of the eye is affected will dictate further localized treatment. Treatment options can include topical lubricants, topical acyclovir gel 5x per day and systemic antiviral +/- topical steroids, as indicated for anterior chamber inflammation. People with HIV infection often require ongoing suppressive antiviral therapy.
Figure 2. Anterior uveitis with keratitic precipitates on the endothelium of the right eye.
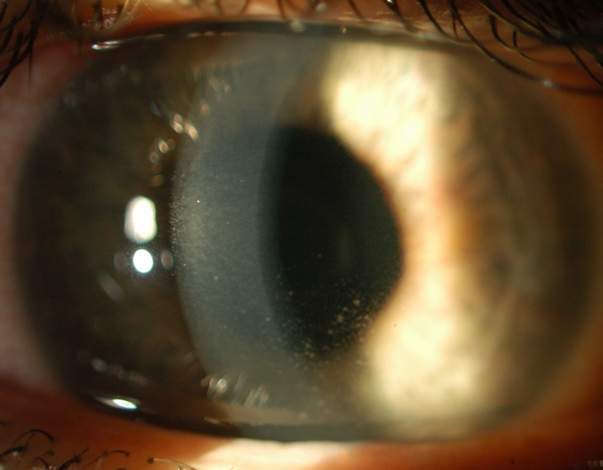
Source: Uveitis Department Sydney Eye Hospital, with permission.
Herpes simplex virus keratouveitis
Herpes simplex virus (HSV) keratouveitis has equal prevalence to the general population in people with HIV infection. HSV is a dsDNA virus with two serotypes. The most common ocular manifestation of HSV infection is a self-limiting blepharoconjunctivitis, characterized by periorbital vesicular rash, follicular conjunctivitis, and preauricular lymphadenopathy. Following this, the virus ascends the sensory nerve axon and, similar to VZV, resides in the trigeminal ganglion from where viral reactivation, replication, and retrograde migration may occur. In the setting of HIV infection, HSV disease of the eye tends to be limbal, more severe, with more recurrences, and dendrites may be larger and less defined compared with HIV seronegative subjects (Figure 3). HIV-infected individuals often require ongoing suppressive antiviral therapy.
Figure 3. Iris transillumination defects and irregular pupil secondary to HSV infection.
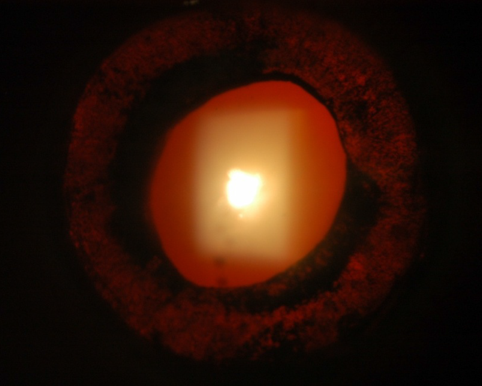
Source: Uveitis Department Sydney Eye Hospital, with permission.
Microsporidiosis
Microsporidia are protozoan obligate intracellular parasites, of which four genera may cause the human disease microsporidiosis. This is usually seen in the immunosuppressed patients (notably in AIDS) where it may present as chronic diarrhoea, respiratory infection, or keratoconjunctivitis. Microsporidial keratouveitis presents with bilateral irritation and photophobia, punctate keratopathy, often with a follicular conjunctivitis and/or an anterior uveitis. Microsporidia are protozoan obligate intracellular parasites, of which four genera may cause the human disease microsporidiosis. It may present as chronic diarrhea or respiratory infection as well as keratoconjunctivitis.
Anterior uveitis
Uveitis may also be caused by concurrent therapy for non-ocular infections, such as Rifabutin for Mycobacterium avium complex infection and Cidofovir for ganciclovir-resistant non-ocular CMV infection, as well as by tuberculosis (TB) and syphilis. Ocular syphilis may present during all stages of disease (primary, secondary and tertiary stages) {ref} Oliver SE, Cope AB, Rinsky JL, Williams C, Liu G, Hawks S, et al. Increases in Ocular Syphilis-North Carolina, 2014-2015. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2017;65(10):1676-82{/ref}. Anterior uveitis is the commonest ocular feature of both secondary and tertiary syphilis. It can be granulomatous or non-granulomatous with variable severity and occasionally roseolae (vascular fronds on the iris) are seen. Iris atrophy and nodules on the iris / iridocorneal angle can occur in tertiary syphilitic uveitis. It is treated (in conjunction with an infectious diseases physician) with systemic antibiotics and topical steroids for the ocular disease {ref}Hoogewoud F, Frumholtz L, Loubet P, Charlier C, Blanche P, Lebeaux D, et al. Prognostic Factors in Syphilitic Uveitis. Ophthalmology. 2017;124(12):1808-16 {/ref}.
Ocular TB can be difficult to diagnose due to its myriad manifestations and the frequent absence of any systemic or radiological evidence of respiratory disease. Clinical features may include lid abscess, conjunctival infiltration/nodules, phlyctenulosis, scleritis (usually anterior necrotizing), interstitial keratitis, granulomatous anterior uveitis with mutton fat Keratic Precipitates (KPs), iris granulomata, Posterior Synechiae (PS) and non-granulomatous anterior uveitis. Ocular TB occurs as a manifestation of disseminated TB in patients with advanced HIV infection and is seen mostly in sub Saharan Africa.

